Maternal Health
Primary Care Utilization and the Health of Adult Women of Childbearing Age in Wisconsin (2024)
The goal of this report is to provide valuable data on adult women of childbearing age (18-44) in Wisconsin, including recent claims data on insured women seen in primary care, as well as electronic health record data on key measures such as depression screening, blood pressure control, and blood sugar control in diabetes.
Taking Action to Reduce Disparities in Adult Women of Childbearing Age
Primary Care Utilization
- Health Center Program
- Primary Care Development Corporation (PCDC)
- Agency for Healthcare Research and Quality
Depression Screening
- What Works for Health: Depression Screening
- The American College of Obstetricians and Gynecologists: Depression During Pregnancy
- Moms Mental Health Initiative
- Equitability of Depression Screening after Implementation of General Adult Screening in Primary Care
Blood Sugar Control in Diabetes
- CDC National Diabetes Prevention Program
- Wisconsin Department of Health Services Chronic Disease Prevention Program: Prediabetes page
- Wisconsin Department of Health Services Chronic Disease Prevention Program: Diabetes page
- Toolkit for Improving Chronic Conditions, Hypertension & Diabetes: Care & Outcomes
- What Works for Health: Diabetes
- March of Dimes: Preexisting Diabetes
- The American College of Obstetricians and Gynecologists: Diabetes and Women
Blood Pressure Control
Priority Measures
Evaluating Change in Health Disparities in Wisconsin: Blood Sugar, Blood Pressure, and Colorectal Cancer Screening (2024)
This report contains recent Wisconsin data that identifies gaps in blood sugar, blood pressure, and colorectal cancer screening across various demographics, including race and ethnicity and rural and urban geography.
Taking Action to Reduce Disparities in Blood Sugar, Blood Pressure, and Colorectal Cancer Screening
Blood Sugar Control in Diabetes
- CDC National Diabetes Prevention Program
- Wisconsin Department of Health Services Chronic Disease Prevention Program: Prediabetes page
- Wisconsin Department of Health Services Chronic Disease Prevention Program: Diabetes page
- Toolkit for Improving Chronic Conditions, Hypertension & Diabetes: Care & Outcomes
- What Works for Health: Diabetes
Blood Pressure Control
- Toolkit for Improving Chronic Conditions, Hypertension & Diabetes: Care & Outcomes
- What Works for Health: Blood Pressure Control
- The Community Guide: Blood Pressure Control
- Quit Connect: A Protocol to Improve Tobacco Quit Line Referrals
- Wisconsin Tobacco Quit Line
Colorectal Cancer Screening
Screening
Disparities in Colorectal Cancer Screening (2022)
Colorectal cancer is the second most common cancer in Wisconsin. Colorectal cancer screening is important because screening tests can help find cancer at an earlier stage, when it may be easier to treat, and identify and remove pre-cancerous polyps before they develop into cancer.
Risk Factors
Disparities in Blood Pressure Control (2022)
Over 30% of Wisconsinites have high blood pressure and only half of those have it under control. Uncontrolled
high blood pressure increases the risk for major cardiovascular disease events, heart disease, stroke, and heart
failure.
Mental Health
Disparities in Mental Health Care and Outcomes (2023)
This report presents recent Wisconsin data on disparities in mental health screening, outpatient visits, and telehealth visits by race and ethnicity, insurance type, age, and rural and urban geography.
Taking Action to Reduce Disparities in Mental Health Care and Outcomes
Resources for Reducing Disparities
- Agency for Healthcare Research and Quality
- National Institute on Minority Health and Health Disparities – Understanding Health Disparities Series
- National Institute on Minority Health and Health Disparities – PhenX Social Determinants of Health Assessments Collection
Mental Health Resources
National Resources
- Centers for Disease Control & Prevention (CDC) Mental Health page
- CDC How Right Now Resource Page
- Lee Thompson Young Foundation – Resources
- National Alliance for Mental Illness (NAMI) Mental Health Education Classes
- National Institute of Mental Health
- National Network to Eliminate Disparities in Behavioral Health (NNED)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- What Works for Health: Mental Health
- HealthExperiencesUSA: Depression in Young Adults
Local Resources
Chronic Disease
Disparities in Diabetes by Geography (2023)
This report examines differences in diabetes management between people with diabetes alone and those with diabetes and cardiovascular disease, while considering whether they live in rural or urban areas.
Disparities in Diabetes Control and Outcomes (2022)
More than 1 in 10 people in Wisconsin have diabetes, and that number continues to grow. Diabetes can lead to serious complications such as heart disease, stroke, amputation, kidney disease, blindness, and death. While disparities pre-date the pandemic, they worsened due to several factors associated with Covid-19. All racial and ethnic groups had lower rates of diabetes control, but American Indian, White, and Black, Wisconsinites had disproportionate drops in primary care visits during the pandemic.
Patient Safety
Disparities in Use of Benzodiazepines and Opioids (2022)
Benzodiazepines for conditions such as anxiety or insomnia and opioids for pain management may lead to safety risks even when only one medication is used. When used at the same time, there is an increased risk of accidents such as falls, and unintentional overdose deaths due to respiratory depression. The CDC recommends that clinicians should avoid prescribing opioids and benzodiazepines at the same time whenever possible. Improving the way opioids and benzodiazepines are prescribed helps patients to recover better or manage longer-term illnesses in a safe manner while reducing these risks.
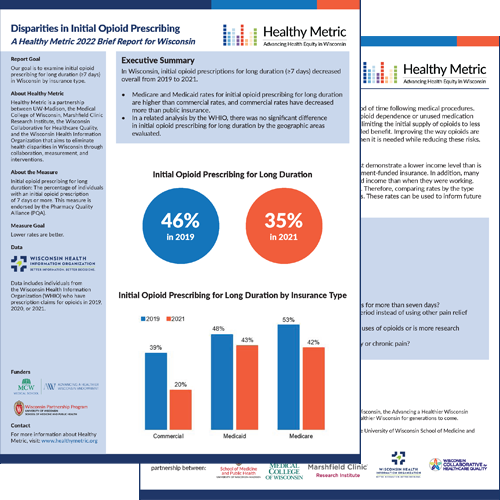
Disparities in Initial Opioid Prescribing (2022)
Millions of Americans require opioids to manage their pain for a short period of time following medical procedures. However, the use of opioids for a longer period may increase the risk for opioid dependence or unused medication that is not properly disposed of. Opioid prescribing guidelines recommend limiting the initial supply of opioids to less than 7 days to decrease the likelihood of physical dependence without added benefit. Improving the way opioids are prescribed helps patients have access to safe, effective pain medication when it is needed while reducing these risks.
